The Safety and Effectiveness of Bio-Identical Hormones: Natural (Bio-Identical) vs. Synthetic HRT
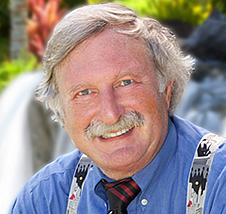
Dr. Holtorf is the Medical Director of the Holtorf Medical Group, Inc, Center for Hormone Imbalance and Fatiguing Conditions in Los Angeles, specializing in CFS, FM, hypothyroidism, chronic illness, and addressing complex endocrine dysfunction. He is board certified and is a Board Examiner for the American Academy of Anti-Aging Medicine.
Below is Dr. Holtorf's review of the medical literature demonstrating how natural hormones are superior to their synthetic counterparts. The conclusion is clear that bio-identical hormones are a safe alternative to Premarin and medroxyprogesterone acetate (MPA), marketed as Provera. The natural bio-identical hormones are very different from their synthetic versions, often having completely opposite physical and cellular effects. Thus, it is critical that women be given the information that these natural hormones do not have the negative side effects of the synthetic hormones and in no way pertain to the conclusions reached by the Women’s Health Initiative (WHI) study. Natural hormones are a safe and more conservative approach to hormone replacement therapy that does not carry the risks associated with Premarin and Provera.
I have found that patients feel great on the natural hormones, but when they are on synthetic hormones, they often do not fully respond or have considerable side-effects. Medical studies confirm that women report improved satisfaction when they are changed from MPA [synthetic progesterone] to natural progesterone and have an improved quality of life.2,50 The medical studies also show that HRT with bio-identical hormones are safer1-79 and far superior to Premarin and Provera with better outcomes and fewer risks and side effects1-79.
The WHI study demonstrated that when MPA was added to Premarin, there was a substantial increase in the risk of heart attack and stroke. This was an expected outcome with MPA, as it has clearly been shown to not only negate any cardioprotective effects of estrogen, but also to actually promote cardiovascular disease and increase the risk of heart attack and stroke.12-17, 34-36, 49-51, 53, 54, 65, 70-73 Natural estrogen and progesterone, on the other hand, have an opposite effect. They maintain and augment the cardioprotective effects of estrogen and decrease the risk of heart attack and stroke.49, 50, 61, 67, 70-72, 76, 77
A number of other medical studies have shown that coronary artery spasm, which increases the risk of heart attack and stroke, can be reduced with estrogen and progesterone,13-15, 68, 69 but the addition of MPA to estrogen has the opposite effect and results in vasoconstriction,13-15, 69 increasing the risk of heart attack and stroke in postmenopausal women. In a study where 18 monkeys had their ovaries removed to simulate menopause, they were then put on estradiol plus either Provera or natural progesterone. After 4 weeks, the researchers injected a substance that causes the coronary arteries to constrict, cutting off the flow of blood to the heart muscle. The researchers reported that the animals receiving Provera would have died within minutes had they not received protective drug therapy. Those on the natural progesterone required no such therapy. The researchers summarized, "We conclude that medroxyprogesterone (Provera) in contrast to progesterone increases the risk of coronary vasospasm."13 This coronary spasm induced by MPA acetate, but not progesterone, results in an increased risk of heart attack and stroke with MPA use but not with natural progesterone use.
Researchers compared the effects of [natural] estrogen and progesterone with estrogen and medroxyprogesterone on exercise induced myocardial ischemia (lowered blood flow) in postmenopausal women with coronary artery disease. This was a blinded randomized crossover study. Women were placed on natural estradiol for four weeks. They were then randomized to receive either natural progesterone or Provera along with the estradiol. After 10 days on the combined therapy the patients then underwent a treadmill test. The patients then crossed over to the opposite therapy and repeated the treadmill test. It was found that exercise time to myocardial ischemia was increased with natural progesterone (decreased risk of heart attack) vs. Provera. They state, "These results imply that the choice of progestin in women at higher cardiovascular risk requires careful consideration." Provera is expected to increase the risk of heart attack and stroke while progesterone is not.14 This coronary dilatation, produced by natural progesterone, but not MPA, increases blood flow to the heart and decreases the risk of heart attack and stroke.
In a series of studies, Adams,51, 61 studied the cardioprotective effects of estrogen and progesterone verses estrogen and MPA. The estrogen and progesterone combination resulted in a 50% reduction in athrosclerotic plaque in the coronary arteries.61 This effect was independent of changes in lipid concentrations. However, when MPA was combined with estrogen, almost all of the cardioprotective effect (athrosclerotic plaque reduction) was reversed and negated.51 MPA was also shown to increase insulin and glucose levels, further increasing the risk of heart disease, heart attack and stroke.51 A number of additional studies have also shown that progesterone by itself76, 77 or in combination with estrogen51, 61, 15 will inhibit athrosclerotic plaque formation. Synthetic progestins, on the other hand, have a completely opposite effect. They promote athrosclerotic plaque formation and inhibit any plaque inhibiting action of estrogen.51, 15, 53, 54 This anti-athrogenic (inhibits plaque formation) effect of progesterone is directly opposite to the effects of synthetic progestins, which is pro-athrogenic (promotes plaque formation). In addition, MPA is unique in that it is shown to increase the amount of collagen in vascular plaques, which promotes thrombus (clot) formation.54, 15 This increases the risk of heart attack, stroke and blood clots. Again, there are significant differences in natural progesterone and synthetic progestins, with the former reducing the risk of heart disease, heart attacks, and strokes, while the latter increases the risk of heart disease, heart attack and stroke.
A review paper by Clarkson, published in the Journal of Reproductive Medicine and entitled Progestogens [term for all progesterone like compounds including progesterone and progestins] and Cardiovascular Disease-A Critical Review, the negative effects of MPA in comparison to progesterone were discussed. The authors summarize, “Of particular interest is the attenuating effect medroxyprogesterone acetate (MPA) has on the cardiovascular benefits of postmenopausal estrogen therapy. MPA reduces the dilatory effect of estrogens on coronary arteries, increases the progression of coronary artery arteriosclerosis, accelerates low-density lipoprotein uptake in plaque, increases the thrombogenic potential of atherosclerotic plaques and promotes insulin resistance and its consequent hyperglycemia. These effects may be largely limited to MPA and not shared with other progestogens.” They boldly display in the middle of the page a summary stating, “The data strongly suggests caution in the use of MPA…” and list as their summary of findings that “These studies, taken together, provide a basis for concern, not about all progestogens, but specifically about MPA.”15 Again, after a review of the literature, it is of no surprise, rather it was expected that the MPA arm of the WHI study would show an increased risk of coronary and cerebral vascular events.
Estrogen and progesterone are superior to estrogen and Provera in the effects on HDL cholesterol. In the large PEPI trial,11 875 postmenopausal women were randomized to receive placebo, Premarin, Premarin and Provera, or Premarin and natural Progesterone. This study demonstrates the superior effect of natural progesterone over Provera. HDL (good cholesterol) was increased by 9% when estrogen and natural progesterone were used versus just a 3-4% increase with estrogen and Provera. The investigators were surprised by the superiority of natural progesterone over synthetic Provera34 with Dr. Healy, a PEPI trial investigator, stating, “I think the biggest surprise certainly was the HDL effect of micronized progesterone. And I quite agree with Dr. Barrett-Connor that any ongoing trial now, whether they be the National Heart, Lung Blood Institute study on estrogen in women who have known coronary disease or the Women’s Health Initiative, should relook at the regimens being offered.” Elizabeth Connor, Cardiologist and PEPI investigator, stated, “If I were treating a women primarily because she was worried about heart disease or because she has dyslipidemia and low HDL cholesterol, I would probably see if she wanted to take micronized [natural] progesterone. I was quite impressed with the better effect.12”
Many experts were surprised when the PEPI trial demonstrated that MPA, but not progesterone, significantly attenuated [blocked] the positive effects of estrogen on lipids. The opposing effects of MPA and progesterone on this cardiovascular risk factor have previously, however, been clearly shown, with MPA and other synthetic progestins negating the positive effects of estrogen on lipids63-65, 70, 72 while progesterone either maintains or augments estrogen’s positive effects on lipids.66, 67, 70-72 Thus, based on their effects on lipids, progesterone would be expected to decrease the risk of heart disease and stroke, while synthetic progestins such as Provera would be expected to increase the risk of heart attack and stroke.
Based on the results from the PEPI Trial and other studies,11, 74 the President of the American Heart Association stated that, just based on this difference in the effects on HDL, a women who changes her medication from MPA to natural progesterone would significantly lower her risk for heart disease.35 The differing effects of progestins [synthetic progesterones] and progesterone on lipids is another risk factor that results in an increased risk for heart disease, heart attack and stroke when the synthetic is used but not natural progesterone.
MPA and synthetic progestins are also shown to significantly increase, even double52, 73, 49, 75 the amount of insulin resistance (Type II diabetes) when compared to estrogen alone or estrogen and progesterone.52, 62, 73, 49 Thus, synthetic progestins are expected to promote vascular disease and increase the risk of heart attack and stroke while natural progesterone does not possess this detrimental effect.
Progesterone was compared to Provera for its ability to decrease the formation of a protein that initiates athrogenic plaques (coronary artery disease), vascular cell adhesion molecule-1. It was shown that progesterone clearly inhibited this protein, but medroxyprogetreone acetate (MPA) (Provera) did not. The authors write, “Because the expression of VCAM-1 is one of the earliest events that occur in the atherogenic process, this adhesion molecule might be the target of progesterone on vascular walls. The contrasting effects of progesterone and MPA seem clinically important, inasmuch as MPA is a widely used progestin in the regimen of hormone replacement therapy.32” This is another process in which MPA promotes heart disease and the risk of heart attack and stroke, while progesterone reduces heart disease and the risk of heart attack and stroke.
Doctor Lignieres, from the Necker Hospital Department of Endocrinology and Reproductive Medicine in Paris, France, reviewed the scientific literature that compared natural oral micronized progesterone and commonly used progestins and published his findings in a 1999 Journal, Clinical Therapeutics. He writes, “The most commonly used synthetic progestins, norethisterone and medroxyprogesterone acetate, have been associated with metabolic and vascular side effects (e.g. suppression of the vasodilating effect of estrogens) in both experimental and human controlled studies. All comparative studies to date conclude that the side effects of synthetic progestins can be minimized or eliminated through the use of natural progesterone.49”
A review of progesterone verses synthetic progestins was done by Fitzpatrick from the department of Internal Medicine at the Mayo Clinic. In this review, entitled "Micronized Progesterone: Clinical Indications and Comparison with Current Treatments," published in Fertility and Sterility, the author summarizes the study’s findings, “A large body of evidence, including the Postmenopausal Estrogen/Progestin Interventions study, suggests that the use of combination estrogen and oral micronized progesterone is optimal for long term hormone replacement therapy. However, use of progesterone-like hormones (progestins) is associated with a number of potential adverse reactions, including bleeding, amenorrhea, and, at higher doses, somnolence. There is also evidence that synthetic progestins have a teratogenic [birth defect] effect when administered during the first 4 months of pregnancy. Therapy with combined estrogen and progestin medication impairs glucose tolerance in some patients.62 The synthetic progestins also may attenuate the beneficial lipid and cardioprotective effects of concomitantly administered estrogen.63, 64 Because of the potential adverse reactions, careful medical oversight is required if the synthetic progestins are to be used during the first trimester of pregnancy or by patients with diabetes, hyperlipidemia, or hypertension. For indications in which oral delivery of synthetic progestins currently are used, the theoretic benefits of oral delivery of the natural form of the hormone are obvious. In addition to the decreased potential for adverse effects, there are clear advantages in convenience, cost, compliance, and quality of life.50”
Premarin, being an oral estrogen, will increase clotting factors and inflammatory proteins, increasing the risk of thromboembolism, stroke and heart attack.16, 18 This does not occur with transdermal estrogens.18 In fact, it can be considered malpractice to give oral contraceptives or oral HRT to smokers because of the increased risk of stroke, but non-smokers are at increased risk, as well. When oral Premarin is taken with Provera the risk of thromboembolism, stroke and heart attack increase in a synergistic manner. Ninety percent of my patients are on transdermal natural estrogens for this reason.18
The Nurses Health Study followed 58,000 postmenopausal women for 16 years (725,000 person-years). The study found that, compared with women who never used hormones, use of unopposed postmenopausal estrogen from ages 50 to 60 years increased the risk of breast cancer to age 70 by 23%. The addition of a progestin to the estrogen replacement resulted in a tripling of the risk of breast cancer to a 67% increase in the risk of breast cancer.78, 9
A large study compared the risk of breast cancer in 1,897 women on combined estrogen and progestin versus 1,637 controls that had never used any HRT. It was found that the use of progestin increased the risk of breast cancer by 38%. The authors conclude, “This study provides strong evidence that the addition of a progestin to HRT enhances markedly the risk of breast cancer relative to estrogen use alone.10” Again, natural progesterone is documented to reduce the risk of breast cancer.
Premarin is made from pregnant horses’ urine, hence its name Pre (pregnant)-mar (horse)- in (urine). It consists of a combination of conjugated equine (horse) estrogens that are more potent and more carcinogenic than other natural estrogens such as estradiol and especially estriol. 4-hydroxyequilenin, a component of Premarin, is especially potent, 100 times the potency of natural estrogen, and carcinogenic.20-22, 80 One author summarizes, “These results suggest that 4-hydroxyequilenin has the potential to be a potent carcinogen through the formation of variety of DNA lesions in vivo.22” Natural estrogens have no such carcinogenic metabolites.
The natural estrogen, estriol, is shown to cause much less breast cell proliferation and is felt to be a much safer form of estrogen than even estradiol and especially Premarin.23-26, 39 Estriol is shown to decrease the incidence and inhibit breast cancer in rats,24, 39, 26 while the levels of estriol in a women are inversely correlated with the risk of breast cancer, with low levels being associated with cancer while high levels are protective.25, 26, 56, 57, 59, 60 An analysis of 6 epidemiologic studies of estrogen levels in women found that there are higher estriol levels in populations with lower risks for breast cancer.26
Dr. Follingstad published an article in the Journal of the American Medical Association, titled "Estriol, the forgotten estrogen?" He reviewed a study in which estriol was given to postmenopausal women with breast cancer. Thirty-seven percent of the patients demonstrated remission or arrest of the disease. He concluded that estriol should be given to all women who need estrogen replacement therapy but are at risk for breast cancer. A case can be made that all women are at risk and estriol should be part of all HRT regimens. He writes, “Enough presumptive and scientific evidence has been accumulated that we may say that orally administered estriol is safer than estrone or estradiol…let us have the estrogen that causes the least risk.27”
In a large study that looked at the effect of estrogens on breast cancer in rats, it was shown that estriol was protective. The authors felt that “The superior protective action of estriol may be partly related to its greater solubility in plasma and decreased binding to plasma-albumin, compared to oestrone [estrone] or 17B-oestradiol [estradiol]58” Premarin on the contrary increases the risk of breast cancer.20-22, 80
There has been considerable research in estrogen metabolism and its relation to breast cancer. Estradiol can be metabolized to either a potent carcinogenic compound, 16-hydroxyestrone, or to a noncarcinogenic compound, 2-hydroxyestrone. Women who metabolize estradiol to 16-hydroxyestrone have a significantly increased risk for breast cancer, and it is being realized that these metabolites likely play a major role in the incidence of breast cancer.40-48 In a study by Kabat et al, entitled "Urinary Estrogen Metabolites and Breast Cancer: A Case Controlled Study," it was found that postmenopausal women with the highest levels of 16-hydroxyestrone compared to 2-hydroxyestrone were shown to have a risk factor for breast cancer that was 32 times that of controls. I routinely check these levels in women and determine the ratios because they have a profound effect on breast cancer risk. Interestingly, women with family histories of breast cancer will usually have elevated 16-hydroxyestrone. If an increased level of the carcinogenic estrone is present, measures are taken to reverse this metabolization pattern and then the levels are re-checked. Estriol, however, does not convert to the carcinogenic 2-hydroxyestrone, making it a much a safer form of estrogen.
Estriol also improves multiple sclerosis while other estrogens make it worse; another indication of its profoundly different effects.28, 29
A number of studies demonstrate that synthetic progestins, such as Provera, increase breast cell proliferation,4, 5, 7, 9, 33, 79, 19, 81 making it pro-carcinogenic and increases the risk of breast cancer.6, 78, 9, 10, 55, 19 This cell proliferation with Provera has been shown to be particularly bad.7 This increased cell proliferation, as expected, translates into an increased risk of breast cancer with medroxyprogesterone use. Natural progesterone, as opposed to medroxyprogsterone, has a strong anti-proliferate effect on breast tissue.1, 8, 81 This is the opposite effect of Provera and results in a strong anti-breast cancer effect of natural progesterone,30, 31, 1, 8 again opposite of Provera.
A double-blind placebo controlled study looked at the effects of estrogen and progesterone on women prior to breast surgery. Patients were given a placebo, estrogen, or estrogen and progesterone for 10-13 days prior to breast surgery. Estradiol increased cell proliferation rates by 230%, but progesterone decreased cell proliferation rates by 400%. The progesterone, when given with estradiol, inhibited and prevented any breast proliferation (cancer preventive).1 Progestins do not have this beneficial effect.
In a double-blind randomized study, Foidart et al also showed that progesterone eliminated estrogen produced breast cell proliferation,8 demonstrating the strong anti-proliferative and anti-cancer effect of natural progesterone. This effect is opposite of that of synthetic progestins, which increase proliferation and increase the risk of breast cancer.4, 5, 7, 9, 33, 78, 79, 19
A prospective epidemiological study conducted at Johns Hopkins demonstrated the profound anti-breast cancer action and protective role of natural progesterone against breast cancer. In that study, 1,083 women who had been evaluated and addressed for infertility were followed for 13 to 33 years. The results showed that the risk of breast cancer was 5.4 times in subjects who had a low progesterone level when compared to those with a normal level. This was particularly striking because the result was so significant despite the fact that the high progesterone group actually had significantly more risk factors for breast cancer than the low progesterone group, indicating that the progesterone level is a far more important parameter. Additionally, women in the low progesterone group experienced 10 times more deaths from neoplasm (cancer) when compared to those with normal progesterone.30
In another study, the protective effect of progesterone or Tamoxifen, a potent estrogen antagonist, was investigated in estrogen-induced breast cancer in rats. Results of the study indicated that the induction rate, multiplicity, and size of estrogen induced mammary tumors were reduced by simultaneous administration of either Tamoxifen or progesterone.31 Natural progesterone is also shown to reduce the number of estrogen receptors in breast tissue (anti-cancer effect).3
These studies indicate that, with respect to the risk of breast cancer, heart disease, heart attacks and stroke, natural hormones offer a safe and more conservative approach to HRT. A large amount of scientific evidence overwhelmingly demonstrates that natural hormones are safer than the study drugs of the WHI, Premarin and Provera. Unfortunately, the overwhelming majority of women do not know that there are safe alternatives to their current HRT or to the one they stopped after the results of the WHI were released. As you can see, it is clear that the negative outcome of the WHI study with the use of MPA is certainly of no surprise, given its clear history of having a negative impact on almost every risk factor for heart disease. Natural progesterone has just an opposite effect of MPA on almost every cardiac risk factor, with MPA increasing the risk of heart attack and stroke, while progesterone decreases the risk. If progesterone was used in the trial, the results would assuredly have been different and their results in no way pertain to natural hormones, which are a safe choice with significantly less risk.
The same is true of the increased incidence of breast cancer demonstrated in the study with the use of Premarin and MPA. This in no way pertains to the use of the natural hormones, estriol and progesterone, which both decrease the risk of breast cancer. The public, and also doctors, need to be told that there is a safer alternative to Premarin and Provera and that HRT [Hormone Replacement Therapy] should not be abandoned based on the results of a known toxic drug combination. It is the utmost importance for women to understand that they have alternatives to Premarin and Provera that are scientifically shown to be safer and healthier.
Selected References
1. Chang HJ, Lee TTY et al. Influences of percutaneous administration of estradiol and progesterone on human breast epithelial cell cycle in vivo. Fertil Steril. 1995;63:785-791.
2. Fitzpatrick La et al. Comparison of regimens containing oral micronized progesterone of medroxyprogesterone acetate on quality of life in postmenopausal women: a cross-sectional survey. J Womens Health Gen Based Med 2000 Mayu;9(4):381-7
3. Gompel et al. Antiestrogen action of progesterone in breast tissue. Breast cancer Res Treat 1986;8(3):179-88.
4.Van der Burg et al. Effects of progestins on the proliferation of estrogen-dependent human breast cancer cells under growth factor-defined conditions. J Steroid Biochem Mol Biol 1992 Jun;42(5):457-65.
5. Mol JA; van Garderen E; Rutteman GR; Rijnberk A. New insights in the molecular mechanism of progestin-induced proliferation of mammary epithelium: induction of the local biosynthesis of growth hormone (GH) in the mammary glands of dogs, cats and humans. J Steroid Biochem Mol Biol 1996 Jan;57(1-2):67-71.
6. Hulka BS, Links between hormone replacement therapy and neoplasia. Fertil Steril 1994 Dec;62(6 Suppl 2):168S-175S.
7. Hofseth LJ; Raafat AM; Osuch JR; Pathak DR; Slomski CA; Haslam SZ Hormone replacement therapy with estrogen or estrogen plus medroxyprogesterone acetate is associated with increased epithelial proliferation in the normal postmenopausal breast. J Clin Endocrinol Metab 1999 Dec;84(12):4559-65.
8. Foidart JM; Colin C; Denoo X; Desreux J; Beliard A; Fournier S; de Lignieres B. Estradiol and progesterone regulate the proliferation of human breast epithelial cells. Fertil Steril 1998 May;69(5):963-9
9. Colditz GA; Rosner B Cumulative risk of breast cancer to age 70 years according to risk factor status: data from the Nurses' Health Study. Am J Epidemiol 2000 Nov 15;152(10):950-64
10. Ross RK; Paganini-Hill A; Wan PC; Pike MC. Effect of hormone replacement therapy on breast cancer risk: estrogen versus estrogen plus progestin. J Natl Cancer Inst 2000 Feb 16;92(4):328-32.
12. Estrogen Replacement therapy and Heart Disease: A Discussion of the PEPI Trial. Women’s Health Information Center.
13. Miyagawa K; Rosch J; Stanczyk F; Hermsmeyer K. Medroxyprogesterone interferes with ovarian steroid protection against coronary vasospasm. Nat Med 1997 Mar;3(3):324-7.
14. Rosano GM; Webb CM; Chierchia S; Morgani GL; Gabraele M; Sarrel PM; de Ziegler D; Collins P. Natural progesterone, but not medroxyprogesterone acetate, enhances the beneficial effect of estrogen on exercise-induced myocardial ischemia in postmenopausal women. J Am Coll Cardiol 2000 Dec;36(7):2154-9.
15. Clarkson TB. Progestogens and cardiovascular disease. A critical review. J Reprod Med 1999 Feb;44(2 Suppl):180-4
16. Feeman WE. Thrombotic stroke in an otherwise healthy middle-aged female related to the use of continuous-combined conjugated equine estrogens and medroxyprogesterone acetate. J Gend Specif Med 2000 Nov-Dec;3(8):62-4; discussion 64-5.
17. Sitruk-Ware R. Progestins and cardiovascular risk markers. Steroids 2000 Oct-Nov;65(10-11):651-8.
18. Scarabin PY; Alhenc-Gelas M; Plu-Bureau G; Taisne P; Agher R; Aiach M. Effects of oral and transdermal estrogen/progesterone regimens on blood coagulation and fibrinolysis in postmenopausal women. A randomized controlled trial Arterioscler Thromb Vasc Biol 1997 Nov;17(11):3071-8
19. Colditz Ga. Hormones and breast cancer: evidence and implications for consideration of risks and benefits of hormone replacement therapy. J Womens Health 1999 Apr;8(3):354-7.
20. Zhang F; Chen Y; Pisha E; Shen L; Xiong Y; van Breemen RB; Bolton JL. The major metabolite of equilin, 4-hydroxyequilin, autoxidizes to an o-quinone which isomerizes to the potent cytotoxin 4-hydroxyequilenin-o-quinone. Chem Res Toxicol 1999 Feb;12(2):204-13.
21. Pisha E; Lui X; Constantinou AI; Bolton JL Evidence that a metabolite of equine estrogens, 4-hydroxyequilenin, induces cellular transformation in vitro. Chem Res Toxicol 2001 Jan;14(1):82-90
22. Zhang F; Swanson SM; van Breemen RB; Liu X; Yang Y; Gu C; Bolton JL. Equine estrogen metabolite 4-hydroxyequilenin induces DNA damage in the rat mammary tissues: formation of single-strand breaks, apurinic sites, and stable adducts, and oxidized bases. Chem Res Toxicol 2001 Dec;14(12):1654-9
23. Tzingounis VA; Aksu MF; Greenblatt RB Estriol in the management of the menopause JAMA 1978 Apr 21;239(16):1638-41.
24. Lemon HM; Kumar PF; Peterson C; Rodriguez-Sierra JF; Abbo KM Inhibition of radiogenic mammary carcinoma in rats by estriol or tamoxifen. Cancer 1989 May 1;63(9):1685-92.
25. Lemon HM; Wotiz HH; Parsons L; Mozden PJ Reduced estriol excretion in patients with breast cancer prior to endocrine therapy. JAMA 1966 Jun 27;196(13):1128-36.
26. Lemon, H.M. Pathophysiologic considerations in the treatment of menopausal patients with oestrogens; the role of oestriol in the prevention of mammary carcinoma. Acta Endocrinol Suppl 1980 233:17-27. DNH
27. Follingstad AH Estriol, The Forgotten Estrogen. JAMA Jan 2 1978, 239(1) p29-30
28. Kim S; Liva SM; Dalal MA; Verity MA; Voskuhl RR Estriol ameliorates autoimmune demyelinating disease: implications for multiple sclerosis. Neurology 1999 Apr 12;52(6):1230-8.
29. Bansil S; Lee HJ; Jindal S; Holtz CR; Cook SD. Correlation between sex hormones and magnetic resonance imaging lesions in multiple sclerosis. Acta Neurol Scand 1999 Feb;99(2):91-4
30. Cowan LD; Gordis L; Tonascia JA; Jones GS. Breast cancer incidence in women with a history of progesterone deficiency. Am J Epidemiol 1981 Aug;114(2):209-17
31. Inoh A; Kamiya K; Fujii Y; Yokoro K Protective effects of progesterone and tamoxifen in estrogen-induced mammary carcinogenesis in ovariectomized W/Fu rats. Jpn J Cancer Res 1985 Aug;76(8):699-704
32. Otsuki M; Saito H; Xu X; Sumitani S; Kouhara H; Kishimoto T; Kasayama S. Progesterone, but not medroxyprogesterone, inhibits vascular cell adhesion molecule-1 expression in human vascular endothelial cells. Arterioscler Thromb Vasc Biol 2001 Feb;21(2):243-8.
33. Braunsberg HA; Coldham NG; Wong W. Hormonal therapies for breast cancer: can progestogens stimulate growth?. Cancer Lett 1986 Feb;30(2):213-8
34. Effects of estrogen or estrogen/progestin regimens on heart disease risk factors in postmenopausal women. The Postmenopausal Estrogen/Progestin Interventions (PEPI) Trial. The Writing Group for the PEPI Trial. JAMA 1995 Jan 18;273(3):199-208
35. News conference at the American Heart association Annual Meeting, Nov 17, 1994.
36. Hargrove JT, et al. menopausal hormone replacement therapy with continuous daily oral mircronized progesterone. Obstet Gyn 1989;73:606-12.
37. Hargrove, Osteen KG. An alternative method of hormone replacement therapy using the natural sex steroids. Infertile Repro Med Clinics north Am. 1995;6:563-674.DNH
38. Hargrove JT, Eisenberg E. Menopause. Med. Clinics North Am 1995;79:1337-1356.
39. Lemon Hm. Antimammary carcinogenic activity of 17-alpha-ethnyl estriol. Cancer 1987;60:2873-81.
40. Schneider J, Huh MM, Bradlow HL, Fishman J. (1984), Antiestrogen action of 2-hydroxyestrone on MCF-7 human breast cancer cells. J Biol Chem 259:4840-4845.
41. Vandewalle B, Lefebvre J. (1989), Opposite effects of estrogen and catechol estrogen on hormone-sensitive breast cancer cell growth and differentiation. Mol Cell Endocrinol 61:239-246.
42. Bradlow HL, Telang NT, Sepkovic DW, Osborne MP. (1996), 2-hydroxyestrone: the ‘good’ estrogen. J Endocrinol 150:Suppl: S259-S265.
43. Fishman J, Martucci C. (1980), Biological properties of 16alpha-hydroxyestrone: Implications in estrogen physiology and pathophysiology. J Clin Endocrinol Metab 51:611-615. DNH
44. Schneider J, Kinne D, Fracchia A, Pierce V, Anderson KE, Bradlow HL, Fishman J. (1982), Abnormal oxidative metabolism of estradiol in women with breast cancer. Proc Natl Acad Sci ,USA 79:3047-3051.DNH
45. Osborne MP, Bradlow HL, Wong GYC, Telang NT. (1993), Upregulation of estradiol C16 alpha-hydroxylation in human breast tissue: a potential biomarker of breast cancer risk. J Natl Cancer Inst 85:1917-1920.
46. Bradlow HL, Hershcopf RJ, Martucci CP,Fishman J. (1985), Estradiol 16?-hydroxylation in the mouse correlates with mammary tumor incidence and presence of murine mammary tumor virus: A possible model for the hormonal etiology of breast cancer in humans. Proc Natl Acad Sci ,USA 82:6295-6299.
47. Telang NT, Suto A, Wong GY, Osborne MP, Bradlow HL. (1992), Induction by estrogen metabolite 16 alpha-hydroxyetrone of genotoxic damage and aberrant cell proliferation in mouse mammary epithelial cells in culture. J Natl Cancer Inst 82:634-638.
48. Kabat GC, Chang CJ, Sparano JA, Sepkovic DW, Hu XP, Khalil A, Rosenblatt R, Bradlow HL. (1997), Urinary estrogen metabolites and breast cancer: a case-control study. Cancer Epidemiol Biomark Prev 6: 505-509.
49. de Lignieres B. Oral micronized progesterone. Clin Ther 1999. jan;21(1):41-60.
50. Fitzpatrick LA, Good A. Micronized progesterone: clinical indications and comparison with current treatment. Fertil Steril 1999 Sept;72(3):389-97.
51. Adams MR; Register TC; Golden DL; Wagner JD; Williams JK Medroxyprogesterone acetate antagonizes inhibitory effects of conjugated equine estrogens on coronary artery atherosclerosis Arterioscler Thromb Vasc Biol 1997 Jan;17(1):217-21 (ISSN: 1079-5642
52. Wagner JD; Martino MA; Jayo MJ; Anthony MS; Clarkson TB; Cefalu WT. The effects of hormone replacement therapy on carbohydrate metabolism and cardiovascular risk factors in surgically postmenopausal cynomolgus monkeys. Metabolism 1996 Oct;45(10):1254-62
53. Levine RL; Chen SJ; Durand J; Chen YF; Oparil S. Medroxyprogesterone attenuates estrogen-mediated inhibition of neointima formation after balloon injury of the rat carotid artery. Circulation 1996 Nov 1;94(9):2221-7.
54. Register TC; Adams MR; Golden DL; Clarkson TB. Conjugated equine estrogens alone, but not in combination with medroxyprogesterone acetate, inhibit aortic connective tissue remodeling after plasma lipid lowering in female monkeys. Athrioscler Thromb Vasc Biol 1998 Jul;18(7):1164-71.
55. Pike MC, Ross RK. Progestins and menopause: epidemiological studies of risks of endometrial and breast cancers. Steroids 2000;65:659-64.
56. MacMahon B; Cole P; Brown JB; Aoki K; Lin TM; Morgan RW; Woo N. Oestrogen profiles of Asian and North American women. Lancet 1971 Oct 23;2(7730):900-2.
57. Lemon HM. Genetic predisposition to carcinoma of the breast: multiple human genotypes for estrogen 16 alpha hydroxylase activity in Caucasians. J Surg Oncol 1972;4(3):255-73
58. Lemon Hm. Oestriol and prevention of breast cancer. Lancet 1973;march 10:546-7.
59. Bulbrook RD; Swain MC; Wang DY; Hayward JL; Kumaoka S; Takatani O; Abe O; Utsunomiya J. Breast cancer in Britain and Japan: plasma oestradiol-17beta, oestrone and progesterone,and their urinary metabolites in normal British and Japanese women. Eur J Cancer 1976 Sep;12(9):725-35.
60.Speroff L. The breast as an endocrine target organ. Contemp Obst Gyn 1977 9:69-72. DNH
61. Adams MR et al. Inhibition of coronary artery athrosclerosis by 17-beta estradiol in ovariectomized monkeys: Lack of an effect of added progesterone. Arteriosclerosis 1990;10:1051-7.
62. Spellacy WN. A review of carbohydrate metabolism and the oral contraceptives. Am J Obstet Gynecol 1969 Jun 1;104(3):448-60.
63. Tikkanen MJ; Kuusi T; Nikkila EA; Sipinen S. Post-menopausal hormone replacement therapy: effects of progestogens on serum lipids and lipoproteins. A review. Maturitas 1986 Mar;8(1):7-17.
64. Newham HH. Oestrogens and atherosclerotic vascular disease: lipid factors. Baillieres Clin Endo Metab 1993;7:61-93.
65. Lobo RA. The role of progestins in hormone replacement therapy. Am J Obstet Gynecol 1992 Jun;166(6 Pt 2):1997-2004
66. Bolaji II; Grimes H; Mortimer G; Tallon DF; Fottrell PF; O'Dwyer EM. Low-dose progesterone therapy in oestrogenised postmenopausal women: effects on plasma lipids, lipoproteins and liver function parameters. Eur J Obstet Gynecol Reprod Biol 1993 Jan;48(1):61-8.
67. Moorjani S; Dupont A; Labrie F; De Lignieres B; Cusan L; Dupont P; Mailloux J; Lupien PJ. Changes in plasma lipoprotein and apolipoprotein composition in relation to oral versus percutaneous administration of estrogen alone or in cyclic association with utrogestan in menopausal women. J Clin Endocrinol Metab 1991 Aug;73(2):373-9.
68. Minshall RD; Miyagawa K; Chadwick CC; Novy MJ; Hermsmeyer K. In vitro modulation of primate coronary vascular muscle cell reactivity by ovarian steroid hormones. FASEB J 1998 Oct;12(13):1419-29
69. Minshall RD; Stanczyk FZ; Miyagawa K; Uchida B; Axthelm M; Novy M; Hermsmeyer K. Ovarian steroid protection against coronary artery hyperreactivity in rhesus monkeys. J Clin Endocrinol Metab 1998 Feb;83(2):649-59.
70. Fahraeus L; Larsson-Cohn U; Wallentin L. L-norgestrel and progesterone have different influences on plasma lipoproteins. Eur J Clin Invest 1983 Dec;13(6):447-53.
71. Jensen J; Riis BJ; Strom V; Nilas L; Christiansen C. Long-term effects of percutaneous estrogens and oral progesterone on serum lipoproteins in postmenopausal women. Am J Obstet Gynecol 1987 Jan;156(1):66-71.
72. Ottosson UB; Johansson BG; von Schoultz B. Subfractions of high-density lipoprotein cholesterol during estrogen replacement therapy: a comparison between progestogens and natural progesterone. Am J Obstet Gynecol 1985 Mar 15;151(6):746-50.
73. Elkind-Hirsch KE; Sherman LD; Malinak R. Hormone replacement therapy alters insulin sensitivity in young women with premature ovarian failure. J Clin Endocrinol Metab 1993 Feb;76(2):472-5.
74. Bush TL; Barrett-Connor E; Cowan LD; Criqui MH; Wallace RB; Suchindran CM; Tyroler HA; Rifkind BM. Cardiovascular mortality and noncontraceptive use of estrogen in women: results from the Lipid Research Clinics Program Follow-up Study. Circulation 1987 Jun;75(6):1102-9.
75. Godsland IF; Gangar K; Walton C; Cust MP; Whitehead MI; Wynn V; Stevenson JC. Insulin resistance, secretion, and elimination in postmenopausal women receiving oral or transdermal hormone replacement therapy. Metabolism 1993 Jul;42(7):846-53.
76. Morey AK; Pedram A; Razandi M; Prins BA; Hu RM; Biesiada E; Levin ER. Estrogen and progesterone inhibit vascular smooth muscle proliferation. Endocrinology 1997 Aug;138(8):3330-9.
77. Lee WS; Harder JA; Yoshizumi M; Lee ME; Haber E. Progesterone inhibits arterial smooth muscle cell proliferation. Nat Med 1997 Sep;3(9):1005-8.
78. Colditz GA; Hankinson SE; Hunter DJ; Willett WC; Manson JE; Stampfer MJ; Hennekens C; Rosner B; Speizer FE. The use of estrogens and progestins and the risk of breast cancer in postmenopausal women. N Engl J Med 1995 Jun 15;332(24):1589-93.
79. von Schoultz B; Soderqvist G; Cline M; von Schoultz E; Skoog L Hormonal regulation of the normal breast Maturitas 1996 May;23 Suppl:S23-5.
80. Chen Y; Liu X; Pisha E; Constantinou AI; Hua Y; Shen L; van Breemen RB; Elguindi EC; Blond SY; Zhang F; Bolton JL. A metabolite of equine estrogens, 4-hydroxyequilenin, induces DNA damage and apoptosis in breast cancer cell lines. Chem Res Toxicol 2000 May;13(5):342-50
81. Desreux J; Kebers F; Noel A; Francart D; Van Cauwenberge H; Heinen V; Thomas JL; Bernard AM; Paris J; Delansorne R; Foidart JM. Progesterone receptor activation. an alternative to SERMs in breast cancer. Eur J Cancer 2000 Sep;36 Suppl 4:S90-1
Jacob Teitelbaum, M.D. is one of the world's leading integrative medical authorities on fibromyalgia and chronic fatigue. He is the lead author of eight research studies on their effective treatments, and has published numerous health & wellness books, including the bestseller on fibromyalgia From Fatigued to Fantastic! and The Fatigue and Fibromyalgia Solution. His newest book (June 10, 2024) is You Can Heal From Long COVID. Dr. Teitelbaum is one of the most frequently quoted fibromyalgia experts in the world and appears often as a guest on news and talk shows nationwide including Good Morning America, The Dr. Oz Show, Oprah & Friends, CNN, and Fox News Health.
