Migraines - The Role of the Hypothalamus
Hypothalamic Activation in Spontaneous Migraine Attacks
Marie Denuelle, MD; Nelly Fabre, MD; Pierre Payoux, MD; Francois Chollet, MD; Gilles Geraud, MD
Headache. 2007;47(10):1418-1426
Posted 02/06/2008
Abstract and Introduction
Abstract
Background: Migraine sufferers experience premonitory symptoms which suggest that primary hypothalamic dysfunction is a likely trigger of the attacks. Neuroendocrine and laboratory data also support this hypothesis. To date, positron emission tomography (PET) scans of migraine sufferers have demonstrated activation of brainstem nuclei, but not of the hypothalamus.
Objective: To record cerebral activations with H215O PET during spontaneous migraine without aura attacks.
Methods: We scanned 7 patients with migraine without aura (6 females and 1 male) in each of 3 situations: within 4 hours of headache onset, after headache relief by sumatriptan injection (between the fourth and the sixth hour after headache onset), and during an attack-free period.
Results: During the headache we found not only significant activations in the midbrain and pons, but also in the hypothalamus, all persisting after headache relief by sumatriptan.
Conclusion: Hypothalamic activity, long suspected by clinical and experimental arguments as a possible trigger for migraine, is demonstrated for the first time during spontaneous attacks.
From the study discussion: What is the significance of the hypothalamic activation seen with migraine in this study? We propose 2 alternatives. The first is that hypothalamic activation simply reflects the general processing of painful stimuli. The hypothalamus, along with the periaqueductal gray matter and ventral tegmental area, form part of a functional network that controls the autonomic and nociceptive components of pain. The role of hypothalamus in antinociception has been demonstrated in animals experiences.18,19 Few PET studies in humans showed hypothalamic activation during traumatic nociceptive pain,20 angina pectoris,21 chronic facial pain,22 or prolonged painful cold stimulation.23 The second possibility is that the hypothalamic activation observed in our study is more specific. Concerning pain originating from the head, hypothalamic orexigenic mechanisms could play a key role in nociception via modulation of dural nociceptive inputs that are thought to be at the origin of migrainous pain.24 The importance of orexigenic mechanisms is stressed by their role in hypothalamic regulation of feeding, arousal, and interestingly in regulation of autonomic system and subsequently represents the link between pain and other symptoms found in primary headaches. Therefore, hypothalamic involvement in the pathogenesis of migraine could be more specific than just as a component of nociceptive pathways.
Clinical observations have suggested a role for the hypothalamus in the initiation of migraine attacks. Many of the premonitory symptoms seen up to 48 hours before the onset of headache are regulated by the hypothalamus. These symptoms include sleep disturbances,25 changes in wakefulness and alertness,26 changes in mood, craving for food, thirst and fluid retention.27,28 Other arguments for the hypothalamic initiation of migraine attacks are: (a) the circadian rhythmicity of the onset of migraine attacks, with a peak incidence in the early morning,29 (b) the fact that sleep disturbances (insomnia or prolonged sleep) are migraine precipitants,30 and (c) the correlation of hormonal fluctuations with migraine frequency in females.31 Neuroendocrine studies suggest also hypothalamic dysfunction in migraine. Patients with chronic migraine also have abnormal patterns of hormonal secretion, including a diminished nocturnal prolactin peak, increased cortisol levels, and a phase delay in the nocturnal melatonin peak.32 Melatonin levels were also reported to be lower during episodes of headache in patients with episodic or menstrual migraine33,34 and in chronic migraine with insomnia.32
The activation of the hypothalamic and brainstem nuclei persisted after our subjects' headaches had been relieved by sumatriptan. If the hypothalamus acts as a generator of migraine, its activation may continue despite downstream disruption of the nociceptive process by sumatriptan. This may explain the frequent recurrence of migraine attacks when sumatriptan ceases to act on the peripheral trigeminovascular system.1 The persistence of hypothalamus activation after sumatriptan has relieved the pain can also be interpreted instead of the activation of a generator as the persistent activation of an antinociceptive mechanism, or both.
Reference: http://www.medscape.com/viewarticle/568627
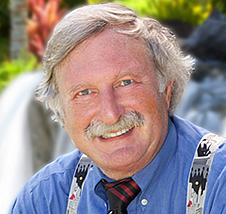
Jacob Teitelbaum, M.D. is one of the most frequently quoted post viral CFS, fibromyalgia, energy, sleep and pain medical authorities in the world. He is the author of 12 books including You Can Heal from Long Covid, the best-selling From Fatigued to Fantastic!, Pain Free 1-2-3, The Complete Guide to Beating Sugar Addiction, Real Cause Real Cure, The Fatigue and Fibromyalgia Solution, and the popular free Smart Phone app Cures A-Z. He is the lead author of eight research studies and three medical textbook chapters on effective treatment for fibromyalgia and chronic fatigue syndrome. Dr. Teitelbaum appears often as a guest on news and talk shows nationwide, including past appearances on Good Morning America, The Dr. Oz Show, Oprah & Friends, CNN, and FoxNewsHealth.
Websites: Vitality101.com | EndFatigue.com
Facebook Support Group: Recovering from Fibromyalgia, Chronic Fatigue, and Long COVID
Facebook Page | Instagram
