Shortness of Breath in CFS/FMS and Post-COVID
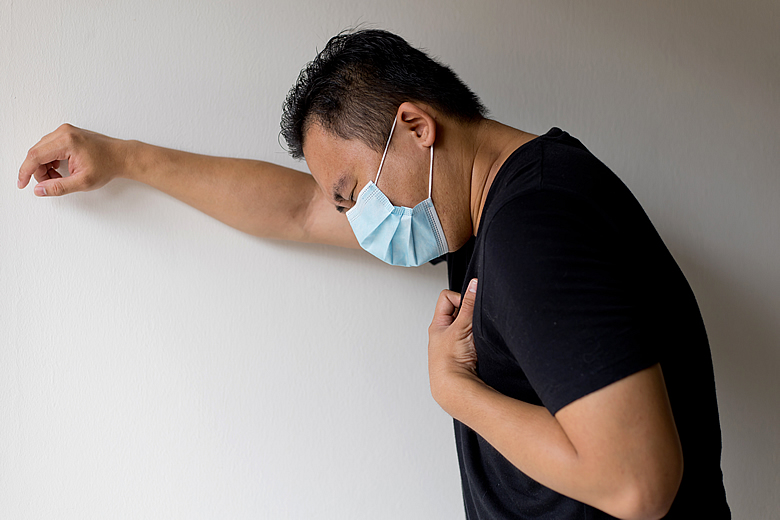
Many people with chronic fatigue syndrome and fibromyalgia suffer with intermittent unexplained shortness of breath. This is becoming especially common with post-COVID.
If you are experiencing this, begin by seeing your family doctor. Unfortunately, most physicians are exceedingly unfamiliar with long COVID or CFS/FMS, so you are only looking for them to rule out heart or lung problems (which medically is straightforward), and any other medical issues they are familiar with. If they aren't able to pinpoint the problem, the information below may help.
Use a Pulse Oximeter
Even before seeing your physician, you can begin to self-examine by using a home pulse oximeter. These are small devices you clip onto your fingertip that can measure your blood oxygen saturation levels, pulse rate and pulse strength. They typically cost $20-$50 and can display results on an LED display in about 10 seconds or so. I would note, however, that there is a lot of variability with how reliable they are. (I bought this one on Amazon and it seems to work fairly well.)
If the pulse oximeter shows an oxygen level of 95% or higher while experiencing shortness of breath, it's unlikley that a serious heart or lung problem is the cause. Especially if you test yourself under exertion and find that your blood oxygen saturation percentage goes up. A reading of 98% or higher suggests a very good probability that you are simply hyperventilating, which can feel very scary but is generally not dangerous.
Other interpretations of the pulse oximeter readout include:
- A percentage oxygen saturation under 95%, especially if it drops with exercise, may suggest heart or lung problems and you should have your doctor rule those possibilities out. This is rarely the issue in those with CFS and FMS, but a little more common in post-COVID.
- If 95-97%, consider the possible causes discussed in the next section.
- If your readout is over 97% when you have shortness of breath, then it is probably hyperventilation.
Let's take a little bit of a deeper dive…
Symptoms Worse with Exertion? Think PEM
After your doctor has ruled out any worrisome heart or lung issues, begin by increasing overall energy production as we discuss below.
Post-exertional malaise (PEM) refers to a worsening of symptoms of CFS/FMS, and now of post-COVID, in which the body perceieves an extreme lack of energy after physical or cognitive exertion that can emerge 24-72 hours after the activity. It often leaves people feeling much worse or even bedbound for the next day or two after the exertion. When this energy "crash" finally resolves, people who've recovered often try to maintain conditioning by continuing to exercise as much as they can, while hoping to avoid a recurrance.
But the real solution to overcoming this condition is to increase overall energy production. And this is just what the S.H.I.N.E.® Protocol does. As anyone who has read my newsletter regularly knows, S.H.I.N.E. is a protocol that identifies five key areas related to the body that, when addressed in combination, provide a research-backed blueprint for promoting optimal energy. These areas include Sleep, Hormones/Hypotension, Immunity/Infections, Nutrition, and Exercise (as able), the details of which are discussed at length in the most recent edition of my book From Fatigued to Fantastic.
Want to Double Your Energy in 1 Minute?
Our recent research and clinical experience suggests as much as a doubling of energy in one minute a day by simply combining the 3 supplements below!
1. Energy Revitalization System™
This simple, low-cost powdered drink mix is IMHO the best multivitamin in the world! It provides 50 key nutrients at opimal levels, replacing over 35 tablets, with 1 good-tasting drink each day. Think I’m kidding? Take a look at its impressive list of ingredients!
This remarkable mix contains ribose, Ashwagandha, Rhodiola, Schisandra, green tea extract, and licorice. 60% of participants in our study reported it gave them an average 62% increase in energy and 90% increase in stamina! (Caution: Licorice can raise blood pressure. Most with FMS have low BP, so no problem. But BP should be monitored in those with high BP.)
3. HRG80™ Red Ginseng Chewable Tablets
In a study we recently published, most reported an average 67% increase in energy with 1 tasty tablet a day. Unfortunately, many other forms of ginseng aren't as effective, as the potent varieties have become nearly extinct.
Live Outside the United States?
Recovery Factors® is available everywhere but the U.S. (efforts are underway to sell in the U.S. soon). Participants in a recent study showed remarkable improvement with this. A 2nd study showing the same is being submitted for publication.
People often ask "What are simple ways to begin to optimize energy?" I have completed four studies on postviral fatigue in the last two years, with some new supplements showing dramatic benefit in increasing energy. I will discuss these studies more in upcoming newsletters.
Other Shortness of Breath Causes
The other key causes of shortness of breath with dropping oxygen saturation post-COVID include:
Decreased Heart Function
This can be seen in CFS/FMS despite a fairly healthy heart. Your heart is a muscle that with low energy has trouble relaxing, just like the other muscles in your body. This makes it hard to totally keep blood flow steady between beats, making it less efficient.This causes what he has called "small heart" or diastolic dysfunction.
COVID, as well as the vaccine for COVID, can trigger heart muscle inflammation. This myocarditis can usually be picked up by most physicians, and tends to heal on its own over a year or two.
But there are things that can be done in the interim to dramatically improve healthy cardiac efficiency and function. These include the Energy Revitalization System™ vitamin powder, ribose, coenzyme Q10, and acetyl l-carnitine. Give these six weeks to see the full effect. (Other supplements to improve heart muscle efficiency can be found in my smartphone app "Cures A-Z" under "Heart Disease.")
Lung Inflammation
This is quite uncommon in standard CFS and fibromyalgia unless a person has asthma (which is easily picked up by physicians). Post-COVID, when people had pneumonia with their COVID, lung damage or even shock lung (acute respiratory distress syndrome, or "ARDS") is not uncommon. This will tend to reflect as a drop in oxygen saturation on the finger clip pulse oximeter below 95% with exercise.
The good news? Research shows that for most causes of shock lung, the lung damage tends to heal by itself over several years. I suspect that this can be facilitated by turning off the oxidative/inflammatory process triggered by the infection.
In general, I help balance healthy inflammation with a supplement called Curamin® (a unique highly absorbed curcumin, Boswellia, DLPA, and nattokinase) 1-2 tablets 1-3 times a day. One study showed that the curcumin also improved energy post-COVID. If people also have widespread discomfort, Curamin will often help that too (after about six weeks). In more severe cases, I also add Clinical Glutathione 1 tablet twice a day for its profound oxidative free radical healing effect.
There is also a lot that can be done in terms of lifestyle and diet as well to decrease inflammation. For this, see my recent post, "Autoimmune and Inflammatory Problems Are Optional."
In cases of very severe lung inflammation, some pulmonary and holistic specialists will use the medication colchicine as well. But that is controversial (albeit reasonable), and beyond the scope of this article.
Normal or Elevated Oxygen Levels, and Shortness of Breath Is Nonexertional
These often are present post-COVID. Symptoms include:
- Hyperventilation and panic attacks.The hallmark symptom is a feeling that you can't take a big enough breath. A full breath is 10 times as big as a normal breath. But in hyperventilation a full breath can feel like little a tiny breath and is associated with anxiety, numbness and tingling going all the way around your lips. It's also associated with lightheadedness, and a feeling like you're going to die. It isn't dangerous, but it's very frightening. There is a lot of information online on how to treat it. Over time, breathing and calming exercises can be especially helpful.
- Vagal nerve inflammation. Nested in the control center of the brain are two key parts of our body's regulatory system. The first, called the sympathetic nervous system, regulates our adrenaline output. The second is a calming part and is called the parasympathetic nervous system. In medical school, we called this the "'old man after dinner" effect. It counterbalances adrenaline and calms the person, predominantly through a major nerve called the vagal nerve.
In a small study of 22 people with long hauler post-COVID, 27% of participants showed evidence of inflammation of the vagal nerve. This shows one more mechanism, in addition to limbic and hypothalamic dysfunction, that contributes to the sense of adrenaline overdrive and POTS that many people with CFS and fibromyalgia have.
Vagal nerve inflammation can be associated with decreased movement of the diaphragm muscle that separates the lungs from the abdomen. This may also be a factor contributing to the sense of breathlessness that many people have. It is generally not dangerous.
"The Anxiety Coach," Dave Carbonell, explains a technique using belly breathing to help decrease the sense of breathlessness.
Another excellent technique called "ANS Rewire", by Dan Neuffer, can reset the entire autonomic nervous system, helping the POTS as well as the racing heart, fatigue, and many of the symptoms seen in CFS/FMS and long COVID.
Other Helpful Treatments for CFS/FMS and Long Haulers
Other treatments helpful to those with CFS/FMS and Long COVID who are experiencing shortness of breath include:
Low-Dose Naltrexone
This compounded medication can be very good for the entire CFS and fibromyalgia process, and likely for Long COVID, along with many other immune mediated conditions. The usual dose is 3-4.5 mg at bedtime and it is routinely made by compounding pharmacies. It takes 8-10 weeks to start working. For more information, visit LowDoseNaltrexone.org, or see my book From Fatigued to Fantastic.
Acupuncture
An excellent study over 25 years ago by the acupuncturist and physician Neoh Aum Choo, MD, showed that three acupuncture points at the base of the skull on each side could relieve this sense of breathlessness in fibromyalgia. Other acupuncture treatments can also be helpful for shortness of breath in general.
Shortness of Breath Usually Not Dangerous
Shortness of breath from any cause can be frightening. Fortunately, most often in CFS, fibromyalgia, and even post-COVID, it does not represent anything dangerous. A simple pulse oximeter will usually distinguish when there is reason for concern, and even then, it is very treatable. Fortunately, knowledge can be a powerful tool toward healing and feeling better.
Jacob Teitelbaum, M.D. is one of the most frequently quoted post viral CFS, fibromyalgia, energy, sleep and pain medical authorities in the world. He is the author of 12 books including You Can Heal from Long Covid, the best-selling From Fatigued to Fantastic!, Pain Free 1-2-3, The Complete Guide to Beating Sugar Addiction, Real Cause Real Cure, The Fatigue and Fibromyalgia Solution, and the popular free Smart Phone app Cures A-Z. He is the lead author of eight research studies and three medical textbook chapters on effective treatment for fibromyalgia and chronic fatigue syndrome. Dr. Teitelbaum appears often as a guest on news and talk shows nationwide, including past appearances on Good Morning America, The Dr. Oz Show, Oprah & Friends, CNN, and FoxNewsHealth.
Websites: Vitality101.com | EndFatigue.com
Facebook Support Group: Recovering from Fibromyalgia, Chronic Fatigue, and Long COVID
Facebook Page | Instagram
